Search
- Page Path
- HOME > Search
- Thyroid
- Hashimoto Thyroiditis and Mortality in Patients with Differentiated Thyroid Cancer: The National Epidemiologic Survey of Thyroid Cancer in Korea and Meta-Analysis
- Injung Yang, Jae Myung Yu, Hye Soo Chung, Yoon Jung Kim, Yong Kyun Roh, Min Kyu Choi, Sung-ho Park, Young Joo Park, Shinje Moon
- Endocrinol Metab. 2024;39(1):140-151. Published online January 3, 2024
- DOI: https://doi.org/10.3803/EnM.2023.1748
- 1,036 View
- 52 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
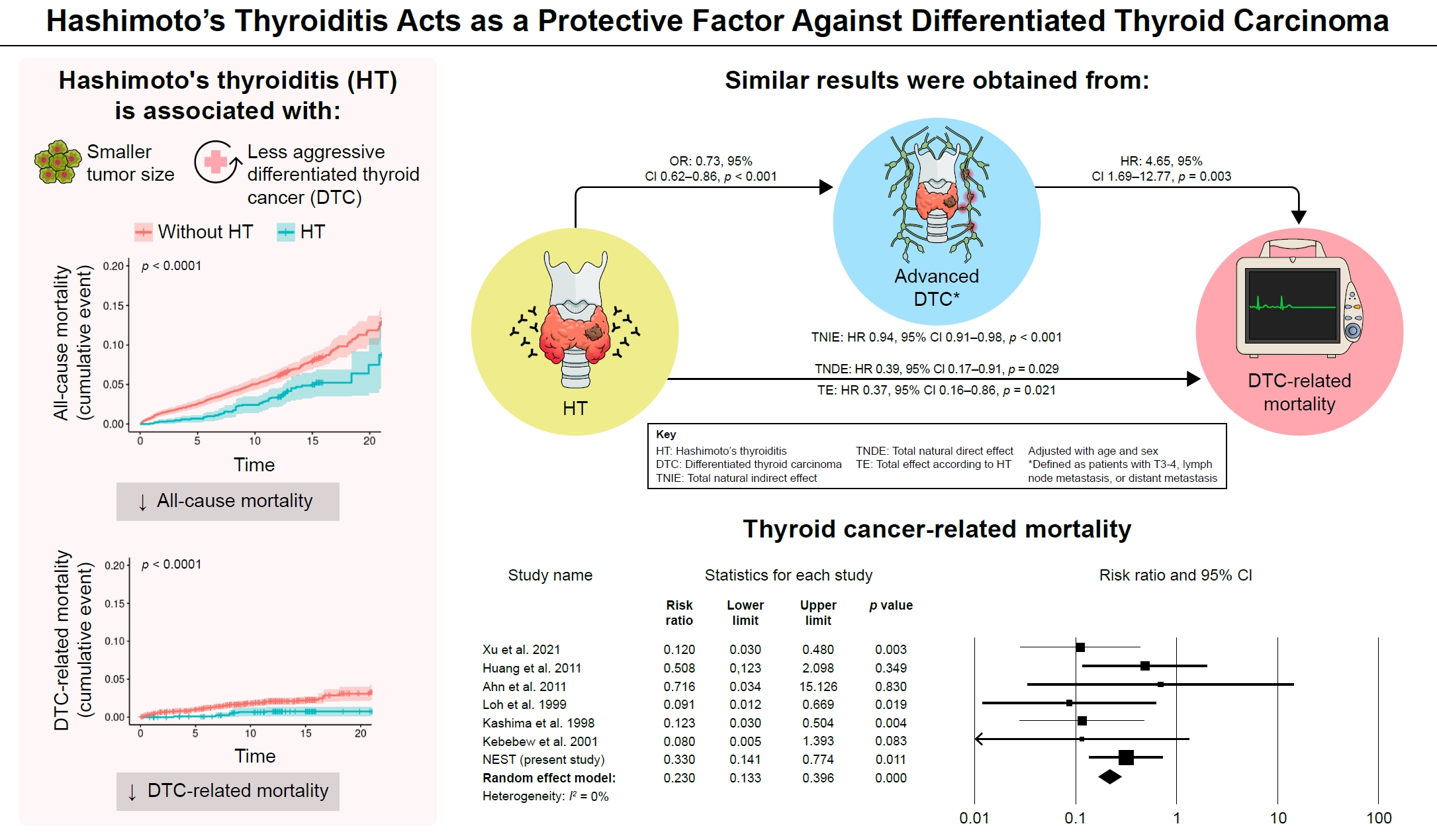
Many studies have shown that Hashimoto’s thyroiditis (HT) acts as a protective factor in differentiated thyroid cancer (DTC), but little is known about its effects on mortality. Therefore, this study was performed to reveal the prognosis of HT on mortality in patients with DTC.
Methods
This study included two types of research results: retrospective cohort study using the National Epidemiologic Survey of Thyroid cancer (NEST) in Korea and meta-analysis study with the NEST data and eight selected studies.
Results
Of the 4,398 patients with DTC in NEST, 341 patients (7.8%) died during the median follow-up period of 15 years (interquartile range, 12.3 to 15.6). Of these, 91 deaths (2.1%) were related to DTC. HT was associated with a smaller tumor size and less aggressive DTC. In Cox regression analysis after adjusting for age and sex, patients with HT showed a significantly lower risk of all-cause death (hazard ratio [HR], 0.71; 95% confidence interval [CI], 0.52 to 0.96) and DTC-related death (HR, 0.33; 95% CI, 0.14 to 0.77). The analysis with inverse probability of treatment weight data adjusted for age, sex, and year of thyroid cancer registration showed similar association. The meta-analysis showed that patients with HT showed a lower risk of all-cause mortality (risk ratio [RR], 0.24; 95% CI, 0.13 to 0.47) and thyroid cancer-related mortality (RR, 0.23; 95% CI, 0.13 to 0.40) in comparison with patients without HT.
Conclusion
This study showed that DTC co-presenting with HT is associated with a low risk of advanced DTC and presents a low risk for all-cause and DTC-related death.

- Diabetes, Obesity and Metabolism
- Efficacy and Safety of the New Appetite Suppressant, Liraglutide: A Meta-Analysis of Randomized Controlled Trials
- Shinje Moon, Jibeom Lee, Hye Soo Chung, Yoon Jung Kim, Jae Myung Yu, Sung Hoon Yu, Chang-Myung Oh
- Endocrinol Metab. 2021;36(3):647-660. Published online June 18, 2021
- DOI: https://doi.org/10.3803/EnM.2020.934

- 6,198 View
- 302 Download
- 13 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity is a chronic disease associated with metabolic diseases such as diabetes and cardiovascular disease. Since the U.S. Food and Drug Administration approved liraglutide as an anti-obesity drug for nondiabetic patients in 2014, it has been widely used for weight control in overweight and obese people. This study aimed to systematically analyze the effects of liraglutide on body weight and other cardiometabolic parameters.
Methods
We investigated articles from PubMed, EMBASE, and the Cochrane Library to search randomized clinical trials that examined body weight changes with liraglutide treatment.
Results
We included 31 studies with 8,060 participants for this meta-analysis. The mean difference (MD) between the liraglutide group and the placebo group was −4.19 kg (95% confidence interval [CI], −4.84 to −3.55), with a −4.16% change from the baseline (95% CI, −4.90 to −3.43). Liraglutide treatment correlated with a significantly reduced body mass index (MD: −1.55; 95% CI, −1.76 to −1.34) and waist circumference (MD: −3.11 cm; 95% CI, −3.59 to −2.62) and significantly decreased blood pressure (systolic blood pressure, MD: −2.85 mm Hg; 95% CI, −3.36 to −2.35; diastolic blood pressure, MD: −0.66 mm Hg; 95% CI, −1.02 to −0.30), glycated hemoglobin (MD: −0.40%; 95% CI, −0.49 to −0.31), and low-density lipoprotein cholesterol (MD: –2.91 mg/dL; 95% CI, −5.28 to −0.53; MD: −0.87% change from baseline; 95% CI, −1.17 to −0.56).
Conclusion
Liraglutide is effective for weight control and can be a promising drug for cardiovascular protection in overweight and obese people. -
Citations
Citations to this article as recorded by- Pharmacotherapy for obesity: moving towards efficacy improvement
Walmir Coutinho, Bruno Halpern
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Physiopathology and Treatment of Obesity and Overweight: A Proposal for a New Anorectic
Bruno Silvestrini, Mauro Silvestrini, Mayank Choubey
Journal of Obesity.2024; 2024: 1. CrossRef - Side effect profile of pharmacologic therapies for liver fibrosis in nonalcoholic fatty liver disease: a systematic review and network meta-analysis
Yilin Li, Rong Lei, Honglin Lei, Qin Xiong, Fengjiao Xie, Chengjiao Yao, Peimin Feng
European Journal of Gastroenterology & Hepatology.2023; 35(1): 1. CrossRef - Recommendations for the prevention and management of obesity in the Iraqi population
Hussein Ali Nwayyir, Esraa Majid Mutasher, Osama Mohammed Alabid, Muthana Abdulrazzaq Jabbar, Wefak Hasan Abdulraheem Al-Kawaz, Haider Ayad Alidrisi, Majid Alabbood, Muhammed Chabek, Munib AlZubaidi, Lujain Anwar Al-khazrajy, Ibtihal Shukri Abd Alhaleem,
Postgraduate Medicine.2023; 135(5): 425. CrossRef - A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - Liraglutide, a glucagon-like peptide-1 analog, in individuals with obesity in clinical practice
Juyoung Shin, Raeun Kim, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 49. CrossRef - The effects of subcutaneous Tirzepatide on obesity and overweight: a systematic review and meta‐regression analysis of randomized controlled trials
Pejman Rohani, Nasser Malekpour Alamdari, Seyedeh Elaheh Bagheri, Azita Hekmatdoost, Mohammad Hassan Sohouli
Frontiers in Endocrinology.2023;[Epub] CrossRef - Efficacy and safety of liraglutide for weight management in children and adolescents: a systematic review and meta-analysis of randomized controlled trials
Hao Gou, Yiman Zhai, Junjun Guo
European Journal of Pediatrics.2023; 182(11): 5095. CrossRef - Efficacy and safety of once-weekly semaglutide in adults with overweight or obesity: a meta-analysis
Ping Zhong, Hai Zeng, Miaochun Huang, Wenbin Fu, Zhixia Chen
Endocrine.2022; 75(3): 718. CrossRef - Pharmacological profile of once-weekly injectable semaglutide for chronic weight management
David C. W. Lau, Rachel L Batterham, Carel W. le Roux
Expert Review of Clinical Pharmacology.2022; 15(3): 251. CrossRef - Pharmacological Management of Obesity: A Century of Expert Opinions in Cecil Textbook of Medicine
Peter Manu, Cristina-Mihaela Lăcătuşu, Liliana M. Rogozea, Simona Cernea
American Journal of Therapeutics.2022; 29(4): e410. CrossRef - GLP-1 agonists: superior for mind and body in antipsychotic-treated patients?
Katerina Horska, Jana Ruda-Kucerova, Silje Skrede
Trends in Endocrinology & Metabolism.2022; 33(9): 628. CrossRef - Targeting skeletal muscle mitochondrial health in obesity
Chantal A. Pileggi, Breana G. Hooks, Ruth McPherson, Robert R.M. Dent, Mary-Ellen Harper
Clinical Science.2022; 136(14): 1081. CrossRef - A Study on Weight Loss Cause as per the Side Effect of Liraglutide
Jin Yu, Jeongmin Lee, Seung-Hwan Lee, Jae-Hyung Cho, Hun-Sung Kim, Heng Zhou
Cardiovascular Therapeutics.2022; 2022: 1. CrossRef
- Pharmacotherapy for obesity: moving towards efficacy improvement

- Camprison of Diagnostic and Therapeutic scans in Patients with Differentiated Thyroid Cancer.
- Yoon Sang Choi, Soo Mi Kim, Shin Gon Kim, Don Hyun Shin, Ie Byung Park, Sei Hyun Baik, Dong Seop Choi, Jae Myung Yu
- J Korean Endocr Soc. 1996;11(4):431-437. Published online November 7, 2019
- 1,312 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Whole body scan using 131-iodine is performed to detect local recurrence or metastasis after thyroidectorny in differenciated thyroid cancer patients. The sensitivity of this procedure is related to the dose of radiopharmaceutical administered. It was reported that 131I posttreatment whole body scan demonstrate foci of tracer uptake not previously observed in diagnostic scan in 10~30% of cases. Posttreatment scans were most likely to reveal new foci in young patients(<45) and patients who had previously received radioactive iodine therapy. Method: We observed the frequency of discordant posttreatment scans and analysed the clicnical significance in 33 differenciated thyroid cancer patients who were admitted for radioiodine ablation from June, 1995 to April, 1996. Results: In 7 cases(21.2%), post treatment scan demonstrated cme or more foci of uptake and revealed less sites of uptake than diagnostic scan in 3 cases(9.1%). In one case with elevated thyroglobulin level and negative diagnostic scan, post treatment scan revealed new uptake sites with thyroid bed and cervical 1ymph node. The sites of discordant uptake were cervical lymph nodes in 4 cases and rnediastinal lymph node in one case, lung in one case, thyroid bed and cervical lymph nodes in one case, 3 cases of 7 pts(43%), demonstrated ane or more foci of uptake in post treatment scan, had history of previous radioiodine treatent. Conclusion: Post treatment scan confirmed uptake into remnant and metaststic tissues identified on the corresponding low dose diagnostic scans. Scanning after high dose radioiodine treatment frequently demonstrated one or more foci of uptake, especially in patients with previous radioiodine treatment, which were not visualized on the diagnostic low dose scan. Treatment scan may be useful for detection of remnant tissue or metastatic lesion in patients with elevated thyroglobulin and negative diagnostic scan.

- Thyroid
- Associations between Hashimoto Thyroiditis and Clinical Outcomes of Papillary Thyroid Cancer: A Meta-Analysis of Observational Studies
- Shinje Moon, Hye Soo Chung, Jae Myung Yu, Hyung Joon Yoo, Jung Hwan Park, Dong Sun Kim, Young Joo Park
- Endocrinol Metab. 2018;33(4):473-484. Published online November 30, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.4.473
- 8,164 View
- 115 Download
- 58 Web of Science
- 55 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Epidemiological studies have suggested an association between Hashimoto thyroiditis (HT) and papillary thyroid cancer (PTC) development. Other studies, however, have reported a protective role of HT against PTC progression. Through this updated meta-analysis, we aimed to clarify the effects of HT on the progression of PTC.
Methods We searched citation databases, including PubMed and Embase, for relevant studies from inception to September 2017. From these studies, we calculated the pooled odds ratios (ORs) of clinicopathologic features and the relative risk (RR) of PTC recurrence with 95% confidence intervals (CIs) using the Mantel-Haenszel method. Additionally, the Higgins
I 2 statistic was used to test for heterogeneity.Results The meta-analysis included 71 published studies with 44,034 participants, among whom 11,132 had HT. We observed negative associations between PTC with comorbid HT and extrathyroidal extension (OR, 0.74; 95% CI, 0.68 to 0.81), lymph node metastasis (OR, 0.82; 95% CI, 0.72 to 0.94), distant metastasis (OR, 0.49; 95% CI, 0.32 to 0.76), and recurrence (RR, 0.50; 95% CI, 0.41 to 0.61).
Conclusion In this meta-analysis, PTC patients with HT appeared to exhibit more favorable clinicopathologic characteristics and a better prognosis than those without HT.
-
Citations
Citations to this article as recorded by- Malignancy risk of indeterminate lymph node at the central compartment in patients with thyroid cancer and concomitant sonographic thyroiditis
Jung Hyo Rhim, Ji Ye Lee, Sun‐Won Park, Younghen Lee, So Lyung Jung, Tae Jin Yun, Eun Ju Ha, Jung Hwan Baek, Jinna Kim, Dong Gyu Na, Ji‐hoon Kim
Head & Neck.2024;[Epub] CrossRef - Hashimoto Thyroiditis and Mortality in Patients with Differentiated Thyroid Cancer: The National Epidemiologic Survey of Thyroid Cancer in Korea and Meta-Analysis
Injung Yang, Jae Myung Yu, Hye Soo Chung, Yoon Jung Kim, Yong Kyun Roh, Min Kyu Choi, Sung-ho Park, Young Joo Park, Shinje Moon
Endocrinology and Metabolism.2024;[Epub] CrossRef - Interaction of BANCR in the relationship between Hashimoto’s thyroiditis and papillary thyroid carcinoma expression patterns and possible molecular mechanisms
Jiabo Zhang, Lingli Yao, Yu Guo
The Journal of Gene Medicine.2024;[Epub] CrossRef - Association between Thyroid Cancer Treatment Outcomes and the Presence of Autoimmune Thyroiditis
Jie Liu
Clinical Thyroidology®.2024; 36(1): 26. CrossRef - Risk prediction for central lymph node metastasis in isolated isthmic papillary thyroid carcinoma by nomogram: A retrospective study from 2010 to 2021
Yu Zhao, Wei Shi, Fang Dong, Xiuhua Wang, Chong Lu, Chunping Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The evaluation of locoregional tumoral involvement in the cooccurrence of hashimoto thyroiditis with papillary thyroid cancer: a case controlled study
Shirzad Nasiri, Seyed Mostafa Meshkati Yazd, Mahsa Gholami, Sepehr Shahriarirad, Sina Sharghi, Reza Shahriarirad
BMC Endocrine Disorders.2023;[Epub] CrossRef - Hashimoto’s Thyroiditis: A Protective Factor against Recurrence in BRAF-Wild Type Differentiated Thyroid Carcinoma
Peter P. Issa, Mahmoud Omar, Yusef Buti, Mohamed Aboueisha, Ruhul Munshi, Mohammad Hussein, Muhib Haidari, Graham Blair, Chad P. Issa, Mohamed Shama, Eman Toraih, Emad Kandil
Cancers.2023; 15(8): 2371. CrossRef - VITAMIN D AND AUTOIMMUNE THYROIDITIS
K. V. Pivtorak, O. V Ivanhuk O. V
Bulletin of Problems Biology and Medicine.2023; 1(1): 44. CrossRef - Does the Association of Hashimoto's Thyroiditis with
Differentiated Thyroid Cancer Really Have a Protective Role?
Ahmet Numan Demir, Zehra Kara, Cem Sulu, Serhat Uysal, Serdar Sahin, Guldana Zulfaliyeva, Oznur Aydin Atar, Nahida Valikhanova, Tulin Ozturk, Hande Mefkure Ozkaya, Mustafa Sait Gonen
Hormone and Metabolic Research.2023; 55(06): 388. CrossRef - Ultrasound, laboratory and histopathological insights in diagnosing papillary thyroid carcinoma in a paediatric population: a single centre follow-up study between 2000-2022
Dominika Januś, Małgorzata Wójcik, Anna Taczanowska-Niemczuk, Aleksandra Kiszka-Wiłkojć, Monika Kujdowicz, Małgorzata Czogała, Wojciech Górecki, Jerzy B. Starzyk
Frontiers in Endocrinology.2023;[Epub] CrossRef - Early Post-operative Stimulated Serum Thyroglobulin: Role in Preventing Unnecessary Radioactive Iodine Treatment in Low to Intermediate Risk Papillary Thyroid Cancer
Havva Sezer, Dilek Yazıcı, Tarık Terzioğlu, Serdar Tezelman, Hande Bulut Canbaz, Aslıhan Yerlikaya, Mehmet Onur Demirkol, Yersu Kapran, Bülent Çolakoğlu, Eda Nur Çilingiroğlu, Faruk Alagöl
The American Surgeon™.2023; 89(12): 5996. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef - Clonal redemption of B cells in cancer
Tyler R. McCaw, Serena Y. Lofftus, Joseph G. Crompton
Frontiers in Immunology.2023;[Epub] CrossRef - Prevalence and Impact of BRAF mutation in patients with concomitant papillary thyroid carcinoma and Hashimoto’s thyroiditis: a systematic review with meta-analysis
Lukasz Janicki, Agastya Patel, Jarosław Jendrzejewski, Andrzej Hellmann
Frontiers in Endocrinology.2023;[Epub] CrossRef - The role of vascular endothelial growth factor in the development of papillary thyroid carcinoma in patients with lymphocytic thyroiditis
Nese E. GULCELIK, Safak AKIN, Kadriye AYDIN, Cisel AYDIN MERICOZ, Yesim G. GULER TEZEL, Aydan USMAN
Minerva Endocrinology.2023;[Epub] CrossRef - Chronic Lymphocytic Thyroiditis and Aggressiveness of Pediatric Differentiated Thyroid Cancer
Richard M. Yeker, Amber D. Shaffer, Pushpa Viswanathan, Selma F. Witchel, Kevin Mollen, Linwah Yip, Sara E. Monaco, Umamaheswar Duvvuri, Jeffrey P. Simons
The Laryngoscope.2022; 132(8): 1668. CrossRef - Bisphenol A drives di(2-ethylhexyl) phthalate promoting thyroid tumorigenesis via regulating HDAC6/PTEN and c-MYC signaling
Xuan Zhang, Nan Guo, Hao Jin, Renqi Liu, Zhen Zhang, Cheng Cheng, Zhijun Fan, Guopei Zhang, Mingyang Xiao, Shengwen Wu, Yuejiao Zhao, Xiaobo Lu
Journal of Hazardous Materials.2022; 425: 127911. CrossRef - Squamous Differentiation in the Thyroid: Metaplasia, Neoplasia, or Bystander?
Meagan A. Chambers, Peter M. Sadow, Darcy A. Kerr
International Journal of Surgical Pathology.2022; 30(4): 385. CrossRef - Vitamin D Implications and Effect of Supplementation in Endocrine Disorders: Autoimmune Thyroid Disorders (Hashimoto’s Disease and Grave’s Disease), Diabetes Mellitus and Obesity
Dorina Galușca, Mihaela Simona Popoviciu, Emilia Elena Babeș, Mădălina Vidican, Andreea Atena Zaha, Vlad Victor Babeș, Alexandru Daniel Jurca, Dana Carmen Zaha, Florian Bodog
Medicina.2022; 58(2): 194. CrossRef - Central Compartment Lymph Nodes Have Distinct Metastatic Patterns in Different Age Groups
Caigu Yan, Xianghui He, Zuoyu Chen, Yizeng Wang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Synchronous occurrence of papillary thyroid microcarcinoma, medullary thyroid carcinoma and Hashimoto thyroiditis in a single thyroid: A case report with literature review
Ari M. Abdullah, Rawa M. Ali, Karzan M. Salih, Karukh K. Mohammed, Fahmi H. Kakamad, Abdulwahid M. Salih
International Journal of Surgery Case Reports.2022; 93: 106888. CrossRef - Benign and malignant thyroid nodules with autoimmune thyroiditis
Georgia N. Kassi, Catherine C. Evangelopoulou, Konstantinos D. Papapostolou, Helen J. Karga
Archives of Endocrinology and Metabolism.2022;[Epub] CrossRef - Association between Hashimoto thyroiditis and clinical outcomes of papillary thyroid carcinoma: A meta-analysis
Qizhi Tang, Weiyu Pan, Liangyue Peng, Francis Moore
PLOS ONE.2022; 17(6): e0269995. CrossRef - A Narrative Review of Preventive Central Lymph Node Dissection in Patients With Papillary Thyroid Cancer - A Necessity or an Excess
David D. Dolidze, Alexey V. Shabunin, Robert B. Mumladze, Arshak V. Vardanyan, Serghei D. Covantsev, Alexander M. Shulutko, Vasiliy I. Semikov, Khalid M. Isaev, Airazat M. Kazaryan
Frontiers in Oncology.2022;[Epub] CrossRef - Role of papillary thyroid carcinoma patients with Hashimoto thyroiditis: evaluation of oxidative stress and inflammatory markers
Natália Medeiros Dias Lopes, Hannah Hamada Mendonça Lens, Walison Augusto da Silva Brito, Julya Karen Bianchi, Poliana Camila Marinello, Rubens Cecchini, André Armani, Alessandra Lourenço Cecchini
Clinical and Translational Oncology.2022; 24(12): 2366. CrossRef - Emerging trends and hot spots in autoimmune thyroiditis research from 2000 to 2022: A bibliometric analysis
Qiuxian Li, Wanyu Yang, Jiashu Li, Zhongyan Shan
Frontiers in Immunology.2022;[Epub] CrossRef - The Immune Landscape of Papillary Thyroid Cancer in the Context of Autoimmune Thyroiditis
Fabiana Pani, Paola Caria, Yoshinori Yasuda, Miyara Makoto, Stefano Mariotti, Laurence Leenhardt, Solmaz Roshanmehr, Patrizio Caturegli, Camille Buffet
Cancers.2022; 14(17): 4287. CrossRef - Comprehensive analysis of lncRNA-mediated ceRNA regulatory networks and key genes associated with papillary thyroid cancer coexistent with Hashimoto’s thyroiditis
Yuepeng Zhang, Yueli Tian
BMC Endocrine Disorders.2022;[Epub] CrossRef - Elastographic Evaluation of Thyroid Nodules in Children and Adolescents with Hashimoto’s Thyroiditis and Nodular Goiter with Reference to Cytological and/or Histopathological Diagnosis
Hanna Borysewicz-Sańczyk, Beata Sawicka, Filip Bossowski, Janusz Dzięcioł, Artur Bossowski
Journal of Clinical Medicine.2022; 11(21): 6339. CrossRef - Prognostic value of the preoperative and early trends in postoperative serum thyroglobulin antibody levels among patients with papillary thyroid carcinoma and concomitant Hashimoto’s thyroiditis
Siyuan Xu, Hui Huang, Jiaxin Qian, Xiaolei Wang, Zhengang Xu, Shaoyan Liu, Jie Liu
Endocrine.2022; 80(2): 392. CrossRef - What has changed in the last 20 years in the postoperative specimen findings of the papillary thyroid cancer cases? A retrospective analysis
Burak Bakar, Pınar Taşar, Turkay Kırdak, Sadık Kılıçturgay
Turkish Journal of Surgery.2022; 38(4): 345. CrossRef - A nomogram model based on the preoperative clinical characteristics of papillary thyroid carcinoma with Hashimoto's thyroiditis to predict central lymph node metastasis
Wanjun Zhao, Linye He, Jingqiang Zhu, Anping Su
Clinical Endocrinology.2021; 94(2): 310. CrossRef - The Association of Histologically Proven Chronic Lymphocytic Thyroiditis with Clinicopathological Features, Lymph Node Metastasis, and Recurrence Rates of Differentiated Thyroid Cancer
Berna İmge Aydoğan, Adile Begüm Bahçecioğlu Mutlu, Seher Yüksel, Sevim Güllü, Rıfat Emral, Özgür Demir, Mustafa Şahin, Vedia Tonyukuk Gedik, Demet Çorapçıoğlu, Serpil Dizbay Sak, Murat Faik Erdoğan
Endocrine Pathology.2021; 32(2): 280. CrossRef - Beneficial autoimmunity improves cancer prognosis
Laurence Zitvogel, Claude Perreault, Olivera J. Finn, Guido Kroemer
Nature Reviews Clinical Oncology.2021; 18(9): 591. CrossRef - Influence Factors for Lymph Node Metastasis in Papillary Thyroid Carcinoma: Hashimoto’s Thyroiditis Has a Weak Effect on Central or Lateral Lymph Node Metastasis
Liguang Zhou, Gang Chen, Lei Sheng, Nan Liu, Bin Zhang, Qingdong Zeng, Bo Chen
Cancer Management and Research.2021; Volume 13: 3953. CrossRef - Implications of a background of Hashimoto’s thyroiditis on the current conservative surgical trend towards papillary thyroid carcinoma
Shadi Hamouri, Sohail Bakkar, Almoutuz Aljaafreh, Mohammed Bani Hani, Hussein Heis, Ghazi Qasaimeh, Nasr Alrabadi, Wisam Al Gargaz, Haitham Odat, Yazan Alkurdi, Tarek Manasreh, Mohammad Matalka, Moamin Badwan
Updates in Surgery.2021; 73(5): 1931. CrossRef - Thyroid nodules in childhood‐onset Hashimoto's thyroiditis: Frequency, risk factors, follow‐up course and genetic alterations of thyroid cancer
Yun Jeong Lee, Yeon Jin Cho, You Joung Heo, Eun‐Jae Chung, Young Hun Choi, Jong‐Il Kim, Young Joo Park, Choong Ho Shin, Young Ah Lee
Clinical Endocrinology.2021; 95(4): 638. CrossRef - Prevalence of Hashimoto Thyroiditis in Adults With Papillary Thyroid Cancer and Its Association With Cancer Recurrence and Outcomes
Siyuan Xu, Hui Huang, Jiaxin Qian, Yang Liu, Ying Huang, Xiaolei Wang, Shaoyan Liu, Zhengang Xu, Jie Liu
JAMA Network Open.2021; 4(7): e2118526. CrossRef - The Effects of Chronic Lymphocytic Thyroiditis on Clinicopathologic Factors in Papillary Thyroid Cancer
Davut Sakiz, Muhammed Erkam Sencar, Murat Calapkulu, Ilknur Ozturk Unsal, Levent Aktas, Bekir Ucan, Mustafa Ozbek, Erman Cakal
Endocrine Practice.2021; 27(12): 1199. CrossRef - Significance of DMBT1 in Papillary Thyroid Carcinoma Concurrent With Hashimoto’s Thyroiditis
Xiao-xiong Gan, Ya-yi Li, Si-jin Li, Shi-sen Mo, Jian-hua Feng, Fei Shen, Wen-song Cai, Ye-qian Lai, Bo Xu
Frontiers in Oncology.2021;[Epub] CrossRef - Pre-existing Thyroiditis Ameliorates Papillary Thyroid Cancer: Insights From a New Mouse Model
Fabiana Pani, Yoshinori Yasuda, Giulia Di Dalmazi, Paulina Chalan, Kathleen Gabrielson, Luigi Adamo, Elena Sabini, Stefano Mariotti, Patrizio Caturegli
Endocrinology.2021;[Epub] CrossRef - Autoimmunity affecting the biliary tract fuels the immunosurveillance of cholangiocarcinoma
Juliette Paillet, Céleste Plantureux, Sarah Lévesque, Julie Le Naour, Gautier Stoll, Allan Sauvat, Pamela Caudana, Jimena Tosello Boari, Norma Bloy, Sylvie Lachkar, Isabelle Martins, Paule Opolon, Andrea Checcoli, Agathe Delaune, Noémie Robil, Pierre de l
Journal of Experimental Medicine.2021;[Epub] CrossRef - Papillary Thyroid Cancer Prognosis: An Evolving Field
Salvatore Ulisse, Enke Baldini, Augusto Lauro, Daniele Pironi, Domenico Tripodi, Eleonora Lori, Iulia Catalina Ferent, Maria Ida Amabile, Antonio Catania, Filippo Maria Di Matteo, Flavio Forte, Alberto Santoro, Piergaspare Palumbo, Vito D’Andrea, Salvator
Cancers.2021; 13(21): 5567. CrossRef - Overexpression of PD-L1 in Papillary Carcinoma and Its Association with Clinicopathological Variables
Servet KOCAÖZ, Gülay TURAN
Düzce Tıp Fakültesi Dergisi.2021; 23(3): 252. CrossRef - Correlation Between Hashimoto's Thyroiditis–Related Thyroid Hormone Levels and 25-Hydroxyvitamin D
Guanqun Chao, Yue Zhu, Lizheng Fang
Frontiers in Endocrinology.2020;[Epub] CrossRef - Oncological impact of hypothyroidism and levothyroxine supplementation following hemithyroidectomy in patients with papillary thyroid carcinoma
Dongbin Ahn, Gil J. Lee, Jin H. Sohn, Jae H. Jeon
Head & Neck.2020; 42(5): 1004. CrossRef - Suspicious ultrasound characteristics correlate with multiple factors that predict central lymph node metastasis of papillary thyroid carcinoma: Significant role of HBME-1
Li Jianming, Liu Jibin, Qian Linxue
European Journal of Radiology.2020; 123: 108801. CrossRef - Unexpected high‐risk pathologic features following thyroidectomy in the chinese immigrant population
Arvind K. Badhey, Erin Moshier, Ameya Jategaonkar, Anni Wong, Kristen Echanique, Raymond L. Chai
The Laryngoscope.2020; 130(7): 1844. CrossRef - Hashimoto's thyroiditis attenuates progression of papillary thyroid carcinoma: deciphering immunological links
Oksana Sulaieva, Oleksii Selezniov, Dmytro Shapochka, Nataliia Belemets, Oleksandr Nechay, Yelizaveta Chereshneva, Dibakhan Tsomartova, Marina Ivanova
Heliyon.2020; 6(1): e03077. CrossRef - Changes in Treg numbers and activity in papillary thyroid carcinoma with and without Hashimoto’s thyroiditis
Na Zhao, Xin Liu, Chao Wu, Yuanchao Liu, Xiangnan Zhao, Xianghui He
Journal of International Medical Research.2020; 48(4): 030006052091922. CrossRef - Genetic relationship between Hashimoto`s thyroiditis and papillary thyroid carcinoma with coexisting Hashimoto`s thyroiditis
Ohoud Subhi, Hans-Juergen Schulten, Nadia Bagatian, Roa'a Al-Dayini, Sajjad Karim, Sherin Bakhashab, Reem Alotibi, Alaa Al-Ahmadi, Manar Ata, Aisha Elaimi, Saad Al-Muhayawi, Majid Mansouri, Khalid Al-Ghamdi, Osman Abdel Hamour, Awatif Jamal, Jaudah Al-Mag
PLOS ONE.2020; 15(6): e0234566. CrossRef - Hashimoto's thyroiditis as a risk factor for thyroid cancer
Ulla Feldt-Rasmussen
Current Opinion in Endocrinology, Diabetes & Obesity.2020; 27(5): 364. CrossRef - Predictive Factors of Recurrence for Multifocal Papillary Thyroid Microcarcinoma With Brafv600e Mutation: A Single Center Study of 1,207 Chinese Patients
Shuai Xue, Li Zhang, Peisong Wang, Jia Liu, Yue Yin, Meishan Jin, Liang Guo, Yuhua Zhou, Guang Chen
Frontiers in Endocrinology.2019;[Epub] CrossRef - Hashimotos’ thyroiditis: Epidemiology, pathogenesis, clinic and therapy
Francesca Ragusa, Poupak Fallahi, Giusy Elia, Debora Gonnella, Sabrina Rosaria Paparo, Claudia Giusti, Leonid P. Churilov, Silvia Martina Ferrari, Alessandro Antonelli
Best Practice & Research Clinical Endocrinology & Metabolism.2019; 33(6): 101367. CrossRef - Características anatomopatológicas del carcinoma papilar de tiroides en especimenes con y sin tiroiditis linfocitica crónica.
Carlos Osorio Covo, Jorge Ballestas Barrera, Jorge Martínez Castro, Zully Acevedo Meza, Diego Barrios Castellar, Francisco Herrera Sáenz, Cesar Redondo Bermúdez, Katherine Redondo De Oro
Revista Ciencias Biomédicas.2019; 8(2): 32. CrossRef
- Malignancy risk of indeterminate lymph node at the central compartment in patients with thyroid cancer and concomitant sonographic thyroiditis

- A Case of Thyrotoxic Periodic Paralysis with Rhabdomyolysis.
- Seo Hee Lee, Seong Yeol Kim, Hae Ri Lee, Jun Goo Kang, Ohk Hyun Ryu, Chul Sik Kim, Byung Wan Lee, Seong Jin Lee, Eun Gyoung Hong, Hyeon Kyu Kim, Doo Man Kim, Jae Myung Yu, Sung Hee Ihm, Moon Gi Choi, Hyung Joon Yoo
- J Korean Endocr Soc. 2008;23(6):425-429. Published online December 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.6.425
- 1,865 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Hyperthyroidism combined with rhabdomyolysis is extremely rare. There are only 6 reported cases of hyperthyroidism accompanied with rhabdomyolysis in the medical literature. Rhabdomyolysis is a syndrome involving the breakdown of skeletal muscle, and this causes myoglobin and intracellular protein to leak into the circulation. The causes of rhabdomyolysis include trauma, electrolyte abnormality, infection, drug, toxin and hypothyroidism. We report here on a patient who presented with thyrotoxic periodic paralysis and rhabdomyolysis with hypokalemia. He complained of lower leg paralysis along with muscle tenderness, and the laboratory findings showed elevated creatine kinase (CK) levels. After treatment by hydration, potassium replacement and drug medication, including propylthiouracil and beta-blocker, his CK levels were normalized and his symptoms were much improved. For patient with thyrotoxic periodic paralysis and muscle tenderness, the possibility of rhabdomyolysis should be clarified by examining the CK levels.

- The Changes in Atherosclerotic Markers and Adiopocytokines after Treatment with Growth Hormone for the Patients with Hypopituitarism and Growth Hormone Deficiency.
- Hyun Won Shin, In Kyung Jeong, Goo Yeong Cho, Cheul Young Choi, Jong Yeop Kim, Yeong Je Chae, Min Ho Cho, Byung Wan Lee, Seong Jin Lee, Chul Young Park, Eun Gyoung Hong, Hyeon Kyu Kim, Doo Man Kim, Jae Myung Yu, Sung Hee Ihm, Moon Ki Choi, Hyung Joon Yoo, Sung Woo Park
- J Korean Endocr Soc. 2006;21(6):515-525. Published online December 1, 2006
- DOI: https://doi.org/10.3803/jkes.2006.21.6.515
- 1,884 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is known that patients with hypopituitarism have a high mortality rate due to the presence of atherosclerosis, cardiovascular diseases and stroke. The aim of this study was the effect of growth hormone (GH) on the atherosclerotic markers and the adipocytokine levels. METHOD: The study was conducted on 13 adult patients with hypopituitarism and growth hormone deficiency (GHD), and they had been stabilized after receiving hormone replacement therapy for other insufficient pituitary hormones, other than GH, for more than one year. Before treatment with GH, we compared the lipid metabolism, glucose metabolism, cardiovascular risk factors and adipocytokine levels, including adiponectin, leptin, TNF-alpha and IL-6, between the GHD patients and 13 healthy adults who were of a similar age and gender distribution. Patients with GHD were treated with 1 U/day of GH for 6 months. We measured insulin-like growth factor-I (IGF-I), blood pressure, body composition, lipid metabolism, glucose metabolism and hs-CRP, cardiac function, adiponectin, leptin, TNF-alpha and IL-6 levels, flow mediated vasodilation (FMD) and nitroglycerin mediated vasodilation (NMD) before and after GH treatment. RESULTS: The patients with hypopituitarism and GHD showed significantly higher levels of total cholesterol (P = 0.002), low-density lipoprotein cholesterol (LDL-C) (P = 0.036), hs-CRP (P = 0.0087) and leptin (P < 0.001) than did the normal healthy adults. However, there was no difference between the normal adults and the patients with GHD for the systolic and diastolic BP, the levels of apoA, apoB, fasting blood glucose(FBG) and HOMA-IR. In the subjects with GHD after treatment with GH, the level of fat mass (P = 0.0017), total cholesterol (P = 0.004), LDL-C (P = 0.001), leptin (P = 0.013), TNF-alpha (P < 0.001) and hs-CRP (P = 0.0001) were significantly reduced, while lean body mass (P = 0.0161), FFA (P = 0.049) and FMD (P = 0.0051) showed a significant increase. However, there was no significant difference in the level of the systolic and diastolic BP, LDL-C, apoA, apoB, LP (a), HOMA-IR, ejection fraction, left ventricular posterior wall, E/A ratio, intraventricular septum, NMD, intima-media thickness, adiponectin, IL-6, FBG and fasting insulin before and after GH treatment. CONCLUSION: The subjects with GHD were vulnerable to cardiovascular disease. GH therapy for 6 months had a positive effect on their various cardiovascular risk factors. -
Citations
Citations to this article as recorded by- Molecular Biology of Atherosclerosis
In-Kyung Jeong
Endocrinology and Metabolism.2010; 25(3): 166. CrossRef
- Molecular Biology of Atherosclerosis

- Duration of Preparation for Postoperative Radioiodine Administration in Differentiated Thyroid Carcinoma.
- Hyeon Kyu Kim, Min Ho Cho, Choel Young Park, Seong Jin Lee, Gi Weon Oh, In Kyung Jeong, Eun Gyung Hong, Sung Hee Ihm, Doo Man Kim, Jae Myung Yu, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park, Jin Hwan Kim, Young Soo Rho
- J Korean Endocr Soc. 2005;20(5):460-466. Published online October 1, 2005
- DOI: https://doi.org/10.3803/jkes.2005.20.5.460
- 1,867 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Radioiodine treatment is effective for the removal of remnant thyroid tissues after thyroidectomy in patients with differentiated thyroid carcinoma. To induce the elevation of serum TSH level which facilitates the uptake of radioiodine into remnants, a 4 to 6 week interval between thyroidectomy and radioiodine administration has been established. During the period of preparation, most patients have experienced overt symptoms of hypothyroidism which have led to the development of alternative strategies. Some reports have suggested that the interval could be reduced to about 3 weeks with less symptoms. We reevaluated the adequate time needed for the elevation of serum TSH level above 30microU/mL after thyroidectomy. METHODS: Forty five patients who had undergone total thyroidectomy for differentiated thyroid carcinoma were investigated. Serum TSH and free T4 levels were measured one or more times within 3 weeks after operation(total 97 blood samples). Eighty nine blood samples were obtained within 15 days. RESULTS: In 41 patients (91.1%) serum TSH levels increased to 30 microU/mL until 15 days after operation. Until postoperative 21 days, serum TSH levels in all the other patients reached 30microU/mL. In linear equation, the daily increment of serum TSH levels was 2.62microU/mL for the first 8 days after operation and 5.34micorU/mL for the next 7 days. The half-life of serum free T4 levels showed marked individual variations. CONCLUSION: Measurement of serum TSH level at about 15 days after total thyroidectomy for differentiated thyroid carcinoma may be useful in determining the time of radioiodine administration.

- A Case of Masked Hypoglycemia during Lactic Acidosis.
- Hee Seon Kim, Ho Sung Yoon, Chang Ok Koh, Hyeon Kyu Kim, Choel Young Park, Seong Jin Lee, Gi Weon Oh, In Kyung Jeong, Eun Gyung Hong, Cheol Soo Choi, Doo Man Kim, Sung Hee Ihm, Jae Myung Yu, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park, Dong Jin Oh
- J Korean Endocr Soc. 2004;19(4):406-410. Published online August 1, 2004
- 1,076 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Severe hypoglycemia induces neuroglycopenic symptoms, including mental alteration, as glucose is the exclusive fuel for the central nervous system. However, some reports have shown that non-glucose fuels, like lactates and ketones, could be utilized by the brain during severe hypoglycemia. Herein, a case of extreme hypoglycemia in a 44-year old woman, subsequently diagnosed as congestive heart failure accompanied by ischemic hepatitis and lactic acidosis, is presented. In two episodes of extreme hypoglycemia, she was fully alert without obvious neurological deficits. In this unusual case, an increased supply of lactate might have maintained the cerebral function and prevented cerebral injury during the hypoglycemia that was induced as a result of starvation and hepatic and cardiac dysfunctions

- The Change of Pulmonary Artery Pressure in Graves'Disease Before and After Treatment.
- Taek Man Nam, Han Soo Cho, Jin Seo Lee, Young Rim Song, Doo Man Kim, Young Cheoul Doo, Cheol Young Park, In Kyung Jeong, Eun Gyung Hong, Seong Jin Lee, Gi Weon Oh, Hyeon Kyu Kim, Jae Myung Yu, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park
- J Korean Endocr Soc. 2003;18(5):465-472. Published online October 1, 2003
- 1,123 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Exertional symptoms, dyspnea and impaired effort tolerance are common in patients with Graves' disease. Proposed explanations include: high-output left heart failure, ineffective oxygen utilization and respiratory muscle weakness. In addition, pulmonary hypertension has also been reported in patients with Graves' disease. A high prevalence of hypothyroidism and positive thyroid autoantibody were also observed in patients with pulmonary arterial hypertension. Therefore, the pulmonary artery pressure in patients with Graves' disease was evaluated. METHODS: Two-dimensional and Doppler echocardiographic examinations (Hewlett Packard Sonos 2500) were performed to determine the pulmonary artery (PA) pressure in 26 Graves' disease patients, both before and after treatment (23 patients with propylthiouracil and 3 with RAI), and in 10 euthyroid controls. The changes in the PA pressure after treatment were evaluated in 13 patients with Graves' disease, who became euthyroid after treatment. RESULTS: The pulmonary artery pressure was increased in the untreated Graves' disease patients compared to the normal controls (23.5+/-2.32 vs. 29.6+/-10.3 mmHg). 38.5% of the Graves' disease patients (10/26) showed pulmonary arterial hypertension (PA>30 mmHg) and the serum TBII levelwas higher in the Graves' disease patients with pulmonary arterial hypertension than in those with normal PA pressure (P<0.05). In the Graves' patients who became euthyroid after treatment, the PA pressure was significantly decreased. CONCLUSION: 38.5% of the untreated Graves' disease patients showed pulmonary arterial hypertension, and the pulmonary artery pressure was significantly decreased in those who became euthyroid after treatment. The pathogenesis and clinical importance of pulmonary arterial hypertension in Graves' disease requires further studies.

- A Case of Cerebral Salt Wasting Syndrome associated with Tuberculous Meningitis.
- Seung Hyuk Rho, Ji Yong Choi, Taek Man Nam, Hyeon Kyu Kim, Seong Jin Lee, In Kyung Jeong, Eun Gyung Hong, Cheol Soo Choi, Doo Man Kim, Jae Myung Yu, Sung Hee Ihm, Moon Gi Choi, Hyung Joon Yoo, Sung Woo Park, Hyoung Cheol Kim
- J Korean Endocr Soc. 2002;17(5):698-704. Published online October 1, 2002
- 1,259 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Hyponatremia in patients with central nervous system disorders is suggestive of the syndrome of inappropriate secretion of antidiuretic hormone (SIADH), and volume restriction is recommended for its correction. However, if volume depletion is present in a situation otherwise compatible with SIADH, cerebral salt wasting syndrome (CSWS) should be considered as the cause of the hyponatremia to avoid hypovolemic shock that may be induced by the standard management of SIADH, i.e. volume restriction. We present a case of a 17-year-old male patient with CSWS associated with tuberculous meningitis. The clinical feature of the patient comprised hyponatremia, excessive natriuresis, polyuria, and hypovolemia. Following the administration of saline and fludrocortisone, natriuresis and polyuria were decreased, and the hyponatremia improved

- Changes in Plasma Dehydroepiandrosterone-Sulfate ( DHEA-S ) Level & DHEA-S / cortisol Ratio by Age in Healthy Korean.
- Jae Myung Yu, Cheol Soo Park, Hyung Joon Yoo, Kwon Yeop Lee, Kyu Yong Park, Cheol Hong Kim, Min Sook Park, Hyun Gyu Kim, Du Man Kim, Sung Hee Ihm, Moon Gi Choi, Sung Woo Park
- J Korean Endocr Soc. 1997;12(2):245-154. Published online January 1, 2001
- 1,088 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
DHEA-S is the most abundant steroid hormone in circulation, and primarily secreted from the adrenal cortex, but its physiological role is little known. One of the characteristic features of DHEA-S is progressive decrement of plasma DHEA-S level with advancing age, in contrast, plasma levels of other adrenal hormones are not chaging or littie decreasing. To grasp the trends of plasma DHEA-S level and DHEA-S/cortisol ratio by age in healthy Korean, we measured the plasma DHEA-S levels and DHEA-S/cortisol ratios in healthy Korean. METHODS: Healthy Korean (men: 99, women: 102, age range: 15-97 year old)were studied. Subjects were not taking drugs (such as glucocorticoid or androgenic medication) or cigarettes known to modify the plasma level of DHEA-S and cortisol, and had no evidence of hepatic, renal disease or hyperlipidemia as determined by serum lipid, bilirubin, SGOT, SGPT, BUN, creatinine. Data were analyzed by 10-year age group for men and women: i.e, 10-19, 20-29, 30-39, 40-49, 50-59, 60-69, 70-79, 80-89 and 90 year or more. Plasma DHEA-S levels were measured by using a commercially available RIA kit with 125I labeled-DHEA-SO4 (Coat-A Count DHEA-SO4), and for the measurement of plasma cortisol levels, commercial Gamma Coat TM[125I] Cortisol Radioimmunassay Kit was used. RESULTS:. 1) In both men and women, plasma DHEA-S level showed high interindividual variation within the same age group. 2) There were individual sex differences in plasma levels of DHEA-S, in all age groups, plasma DHEA-S levels were significantly higher values for men than for women. 3) Maximum plasma DHEA-S levels (men; 237+-3.35 ug/dL, women; 108+-17.5 ug/dL) were at third decade in both men and women. 4) Both men and women showed the continuous decline in plasma DHEA-S level with age. These age-related decline was more prominent in men than in women (men; y=-3.152 * +292.6, r2= 0.8459, P<0.05, women; y= -1.417 * +143.3, r2 = 0.7278, P< 0.05). 5) As an index of aging, there was no stastical difference between DHEA-S and DHEA-S/cortisol ratio. CONCLUSION: In healthy Korean, there were high interindividual variation of plasrna DHEA-S levels. In both men and women plasma DHEA-S level was peak at third decade, and from when it declined progressively with age. These results suggest that although the reliability of single plasma DHEA-S measurement are limited, the decline of DHEA-S with advancing age might be a specific marker of endocrinologic hormonal milieu (aging index). Also, concerning to individual adrenal secreting capacity, we measured DHEA-S/cortisol ratio. But we did not found that plasma DHEA-S/cortisol ratio is superior to the plasma DHEA-S level as an aging index.

- 4 unusual cases of pheochromocytoma.
- Sai Hyun Baik, Kyung Mook Choi, Eun Jong Lee, Yong Hyun Kim, Sang Jin Kim, Jae Myung Yu, Dong Seop Choi
- J Korean Endocr Soc. 1993;8(3):356-362. Published online January 1, 2001
- 1,068 View
- 18 Download

- A case of familial goiter due to organification defect in siblings.
- Sang Jin Kim, Eun Jong Lee, Yong Hyun Kim, Goo Lee, Sai Hyun Paik, Jae Myung Yu, Dong Seop Choi, Jae Geol Choi
- J Korean Endocr Soc. 1992;7(4):391-396. Published online January 1, 2001
- 1,032 View
- 16 Download

- A case of lingual thyroid with euthyroidism.
- Sin Hyung Lee, Yong Hyun Kim, Eun Jong Lee, Sang Jin Kim, Jae Myung Yu, Sei Hyun Baik, Dong Seop Choi
- J Korean Endocr Soc. 1992;7(3):300-304. Published online January 1, 2001
- 1,118 View
- 16 Download


 KES
KES

 First
First Prev
Prev



